Coronary Artery Bypass Graft Surgery
What is coronary bypass graft surgery?
Coronary artery bypass graft surgery (CABG) is a procedure used to treat coronary artery disease. Coronary artery disease (CAD) is the narrowing of the coronary arteries. These are the blood vessels that supply oxygen and nutrients to the heart muscle. CAD is caused by a build-up of fatty material within the walls of the arteries. This buildup narrows the inside of the arteries, limiting the supply of oxygen-rich blood to the heart muscle.
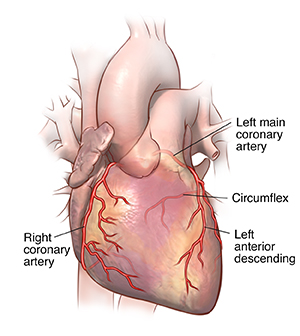
One way to treat the blocked or narrowed arteries is to bypass the blocked portion of the coronary artery with a piece of a healthy blood vessel from elsewhere in your body. Blood vessels, or grafts, used for the bypass procedure may be pieces of a vein from your leg or an artery in your chest. An artery from your wrist may also be used. Your healthcare provider attaches 1 end of the graft above the blockage and the other end below the blockage. Blood bypasses the blockage by going through the new graft to reach the heart muscle. This is called coronary artery bypass surgery.
Traditionally, to bypass the blocked coronary artery, your provider makes a large cut (incision) in the chest and briefly stops the heart. To open the chest, your provider cuts the breastbone (sternum) in half lengthwise and spreads it apart. Once the heart is exposed, your provider inserts tubes into the heart. This lets the blood be pumped through the body by a heart-lung bypass machine. The bypass machine is needed to pump blood while the heart is stopped.
The traditional open heart procedure is still commonly done. In many cases it may be preferred. But less invasive methods have been developed to bypass blocked coronary arteries. Off-pump procedures, in which the heart does not have to be stopped, were developed in the 1990's. Other minimally invasive procedures, such as keyhole surgery (done through very small incisions) and robotic procedures (done with the aid of a moving mechanical device), may be used.
Why might I need coronary artery bypass surgery?
Coronary artery bypass graft surgery (CABG) is done to treat a blockage or narrowing of 1 or more of the coronary arteries. It can restore the blood supply to your heart muscle when nonsurgical procedures are not a choice.
Symptoms of coronary artery disease may include:
You may not have any symptoms in early coronary artery disease. But the disease will continue to progress until there’s enough artery blockage to cause symptoms and problems. If the blood supply to your heart muscle continues to decrease as a result of increasing blockage of a coronary artery, you may have a heart attack. If the blood flow can’t be restored to the part of the heart muscle affected, the tissue dies.
There may be other reasons for your provider to advise CABG surgery.
What are the risks of coronary artery bypass surgery?
Possible risks of coronary artery bypass graft surgery (CABG) include:
-
Bleeding during or after the surgery
-
Blood clots that can cause heart attack, stroke, or lung problems
-
Infection at the incision site
-
Pneumonia
-
Breathing problems
-
Pancreatitis
-
Kidney failure
-
Abnormal heart rhythms
-
Failure of the graft
-
Death
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your provider before the procedure.
How do I get ready for coronary artery bypass surgery?
-
Your healthcare provider will explain the procedure and you can ask questions.
-
You will be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if anything is unclear.
-
Along with a review of your health history, your provider may do a complete physical exam to make sure you are in otherwise good health before having the procedure. You may need blood tests or other diagnostic tests.
-
You will be asked to not eat or drink for 8 hours before the procedure, generally after midnight.
-
You may be asked to shower with a soap or special cleanser the night before and the morning of surgery.
-
Tell your provider if you are pregnant or think you could be.
-
Tell your provider if you are sensitive to or are allergic to any medicines, iodine, latex, tape, or anesthetic medicines (local and general).
-
Tell your provider about all medicines (prescription and over-the-counter), vitamins, herbs, and supplements that you are taking.
-
Tell your provider if you have a history of bleeding disorders or if you are taking any blood-thinning medicines, aspirin, or other medicines that affect blood clotting. You may be told to stop some of these medicines before the procedure. Ask which medicines to take, and which to stop, and when you should stop taking them.
-
You may need blood tests before the procedure to find out how long it takes your blood to clot.
-
Tell your provider if you have a pacemaker, another implanted cardiac device, or any other implants.
-
If you smoke, stop smoking as soon as possible. This may improve your chances for a successful recovery from surgery and benefit your overall health.
-
Based on your medical condition, your provider may ask you to do other things to get ready.
What happens during coronary artery bypass?
Coronary artery bypass graft surgery (CABG) requires a stay in a hospital. Procedure may vary depending on your condition and your healthcare provider's practices.
Generally, CABG follows this process:
-
You will be asked to remove any jewelry or other objects that may interfere with the procedure.
-
You will change into a hospital gown and empty your bladder.
-
A healthcare professional will insert an IV (intravenous) line in your arm or hand. Other catheters will be put in your neck and wrist to monitor your heart and blood pressure, as well as to take blood samples.
-
You will lie on your back on an operating table.
-
The anesthesiologist will continuously keep track of your heart rate, blood pressure, breathing, and blood oxygen level during the surgery. Once you are sedated (put into a deep sleep), a breathing tube will be put into your throat and you will be connected to a ventilator, which will breathe for you during the surgery.
-
A catheter will be put into your bladder to drain urine.
-
The skin over the surgical site will be cleaned with an antiseptic solution.
-
Once all the tubes and monitors are in place, your provider will make cuts in 1 or both of your legs or 1 of your wrists. This is to access the blood vessel(s) to be used for the grafts. They will remove the vessel(s) and close those incision(s).
-
The provider will make a cut down the center of your chest from just above the breastbone to just below where the chest ends.
-
The provider will cut the sternum (breastbone) in half lengthwise. They will separate the halves of the breastbone and spread them apart to expose your heart.
Coronary artery bypass graft surgery, on-pump procedure
-
To sew the grafts onto the very small coronary arteries, your healthcare provider will need to stop your heart temporarily. Tubes will be put into the heart so that your blood can be pumped through your body by a heart-lung bypass machine.
-
Once the blood has been diverted into the bypass machine for pumping, your provider will stop the heart by injecting it with a cold solution.
-
When the heart has been stopped, the provider will do the bypass graft procedure by sewing one end of a section of vein over a tiny opening made in the aorta, and the other end over a tiny opening made in the coronary artery just below the blockage. If your provider uses the internal mammary artery inside your chest as a bypass graft, the lower end of the artery will be cut from inside the chest and sewn over an opening made in the coronary artery below the blockage.
-
You may need more than 1 bypass graft done, depending on how many blockages you have and where they are located. After all the grafts have been completed, the provider will closely check them as blood runs through them to make sure they are working.
-
Once the bypass grafts have been checked, the provider will let the blood circulating through the bypass machine back into your heart and they will remove the tubes to the machine. Your heart may restart on its own, or a mild electric shock may be used to restart it.
-
Your provider may put short-term wires for pacing into your heart. These wires can be attached to a pacemaker. Your heart can be paced, if needed, during the early recovery period.
Coronary artery bypass surgery, off-pump procedure
-
Once your healthcare provider has opened the chest, the area around the artery is stabilized for the bypass.
-
The rest of the heart will continue to function and pump blood through the body.
-
The heart-lung bypass machine and the person who runs it may be kept on stand-by just in case the procedure needs to be completed on bypass.
-
The provider will do the bypass graft procedure by sewing one end of a section of vein over a tiny opening made in the aorta, and the other end over a tiny opening made in the coronary artery just below the blockage.
-
You may have more than one bypass graft done, depending on how many blockages you have and where they are located.
-
Before the chest is closed, the provider will closely examine the grafts to make sure they are working.
Procedure completion, both methods
-
Your provider will sew the sternum together with small wires (like those sometimes used to repair a broken bone).
-
They will insert tubes into your chest to drain blood and other fluids from around the heart.
-
Your provider will sew the skin over the sternum back together.
-
Your provider may put a tube through your mouth or nose into your stomach to drain stomach fluids.
-
They will then apply a sterile bandage or dressing.
What happens after coronary artery bypass surgery?
In the hospital
After the surgery, you may be taken to the recovery room and then the intensive care unit (ICU) to be closely monitored. Machines will constantly display your electrocardiogram tracing, blood pressure, other pressure readings, breathing rate, and your oxygen level. Coronary artery bypass surgery (CABG) requires a hospital stay of at least several days.
You will most likely have a tube in your throat to help with breathing through a ventilator (breathing machine) until you are stable enough to breathe on your own. As you continue to wake up from the anesthesia and start to breathe on your own, your healthcare provider can adjust the breathing machine to allow you to take over more of the breathing. When you are awake enough to breathe completely on your own and you are able to cough, your provider will remove the breathing tube. In most cases, the breathing tube is removed soon after the operation, usually the same day or by early the next morning. Your provider will also remove the stomach tube at this time.
After the breathing tube is out, a nurse will help you cough and take deep breaths every couple of hours. This will be uncomfortable due to soreness, but it's very important that you do this to keep mucus from collecting in your lungs and possibly causing pneumonia. Your nurse will show you how to hug a pillow tightly against your chest while coughing to help ease the discomfort.
The surgical incision may be tender or sore for several days after a CABG procedure. Take a pain reliever for soreness as recommended by your provider. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only recommended medicines.
Your provider may deliver medicines through the IV to help your blood pressure and your heart, and to control any problems with bleeding. As your condition stabilizes, they will gradually decrease and then stop these medicines.
Once your provider removes the breathing and stomach tubes and you are stable, you may start to drink liquids. You can gradually include more solid foods as you can tolerate them. Your nurse will help you sit up on the side of the bed and dangle your feet. If you are able to do this, the nurse will help you sit up for a while in a chair.
When your provider determines that you are ready, you will be moved from the ICU to a postsurgical nursing unit. Your recovery will continue there. You can gradually increase your activity as you get out of bed and walk around for longer periods. This helps prevent complications from the surgery, such as pneumonia or blood clots in your legs. You can eat solid foods as soon as you can tolerate them.
A member of your care team will arrange for you to go home and schedule a follow-up visit with your provider.
At home
Once you are home, it will be important to keep the surgical area clean and dry. Your healthcare provider will give you specific bathing instructions. They will remove the stitches or surgical staples during a follow-up office visit, if they were not removed before leaving the hospital.
Don't drive until your provider tells you it's OK. You may have other activity restrictions.
Call your provider right away if any of these occur:
-
Fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Chills
-
Redness, swelling, or bleeding or fluid leaking from any of the incision sites
-
More pain around any of the incision sites
-
Fast or irregular pulse
-
Leg swellings
-
Arm and leg numbness
-
Lasting nausea or vomiting
Call 911 right away if you have any of these:
Your provider may give you other instructions after the procedure, depending on your situation.
When your recovery time ends, your provider may advise that you start a cardiac rehab (rehabilitation) program. This helps you get back to a normal lifestyle. Cardiac rehab starts in the hospital with simple walking. It goes on to help you with a regular exercise routine and a healthy diet. These healthier habits can prevent heart problems in the future.
Next steps
Before you agree to the test or procedure make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure