Sentinel Lymph Node Biopsy
What is a sentinel lymph node biopsy?
A sentinel lymph node biopsy is a type of surgery done to remove the fewest number of lymph nodes needed to evaluate for cancer metastasis. It helps find out if and how far cancer has spread in the body while reducing side effects of bigger surgeries.
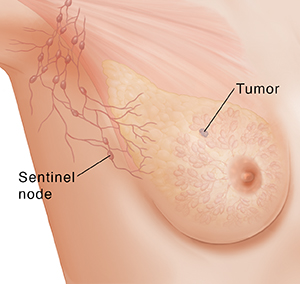
Lymph nodes are part of the body’s lymphatic system. This system helps your body fight infections. A clear fluid called lymph moves through the lymphatic system. It carries infection-fighting white blood cells all through your body and picks up cell waste. The lymph flows to your lymph nodes. Lymph nodes are small, round organs along the lymph vessels. They filter lymph fluid. You have hundreds of them all over your body.
Lymph nodes might become large, firmer, and painful when you have an infection. You might feel them in your neck, underarms, groin, belly (abdomen), and chest. Cancer cells can spread into lymph and be carried to a lymph node. Then the node may swell, feel hard, and might hurt. Or you may not feel it at all.
When you have a cancerous tumor, the sentinel lymph node is the first node or nodes that the cancer cells tend to spread to, before going to other lymph nodes. Looking at cells in the sentinel node(s) can give a lot of information about the cancer. A sentinel lymph node biopsy is a surgery to take out these nodes. Then they can be tested for cancer cells.
Why might I need a sentinel lymph node biopsy?
The main reason for a sentinel lymph node biopsy is to find out if the cancer has spread beyond the main tumor. This will help decide the best treatment for you.
With a sentinel lymph node biopsy, more lymph nodes will be removed if the sentinel nodes have cancer cells in them. If the sentinel nodes don't contain cancer cells, no other nodes are removed. Removing fewer nodes reduces the risk of long-term side effects after surgery.
Whether a sentinel lymph node biopsy can be done depends on the type of cancer and where it is in the body. This type of biopsy is most often used for breast cancer and melanoma. It might also be used for penile and endometrial cancer, and it's being studied for many other kinds of cancer.
What are the risks of a sentinel lymph node biopsy?
All surgery can have harmful side effects. But when fewer nodes are taken out, the risks are less than if a lot of nodes are removed.
The most common risks include:
-
Pain and swelling at the biopsy site
-
Bruising at the biopsy site
-
Swelling from lymph buildup in the area
-
A pocket of lymph fluid (seroma) forming
-
Allergic reaction to the contrast dye used to do the biopsy
-
Short-term changes in urine color or stains on the skin from the dye
There may be other risks, too. These depend on your overall health. Talk with your healthcare provider about your risks and any concerns you have.
How do I get ready for a sentinel lymph node biopsy?
Tell your healthcare provider if you:
-
Are pregnant or think you are pregnant
-
Are taking any medicines, vitamins, supplements, or herbs
-
Use marijuana
-
Use any illegal drugs
-
Have any allergies to anesthesia or dyes
-
Have any bleeding problems
-
Take blood-thinning medicines, like aspirin or warfarin
-
Have had a biopsy in the past
-
Have had radiation treatment to the biopsy site
You will be given anesthesia to make you sleep and not feel pain during the surgery. Follow all directions about when to stop eating and drinking before the surgery. Plan to have someone take you home afterward.
What happens during a sentinel lymph node biopsy?
The biopsy is often done on an outpatient basis. This means you can go home after the procedure. In some cases, you may need to stay overnight. From start to finish, the procedure might take about an hour. It depends on whether it's part of another surgery or the only thing being done. This is how a sentinel lymph node biopsy is usually done:
-
You'll get a sedative to help you relax.
-
You may get local or general anesthesia. Local means the medicines are used to numb the area so you don't feel pain. General anesthesia is when medicines are used to put you into a deep sleep during the surgery.
-
The surgeon will use a needle to inject a radioactive tracer or blue dye into the tumor or the tissue around it. Sometimes both the tracer and dye are used.
-
A scanner is used to find the lymph node or nodes that the radioactive tracer or the blue dye go to first. This is the sentinel lymph node. There can be more than one.
-
The surgeon will make a small cut (incision) in the skin and take out the node(s).
-
The incision is then closed with stitches or glue. It's covered with a bandage until it heals.
What happens after a sentinel lymph node biopsy?
Once the node(s) is removed, it's sent to a lab. There, a pathologist c checks it for cancer.
Based on what the pathologist finds, your healthcare team will outline the rest of your treatment plan. If cancer is found, more lymph nodes need to be removed in a second surgery. Sometimes, the biopsy is planned so the pathologist can check the sentinel node as soon as it's removed. Then, if cancer is found, more lymph nodes can be removed during the same surgery. If no cancer is found, it's unlikely that the cancer has spread to other lymph nodes, so no more lymph node surgery is needed.
After the biopsy, you may feel some pain at the site of the surgery. You may also be drowsy until the medicines wear off. Your healthcare provider will likely give you pain medicine. Pain should get better after a few days. You may have a little bleeding or swelling at the site of the biopsy. This will go away as you heal. Follow all directions from your provider about activity, taking medicine, and caring for the incision site after surgery.
Call your healthcare provider right away if any of the following occur:
-
Increased swelling at the biopsy site
-
An increase in pain or redness at the site
-
Increased bleeding from the site
-
Pus or drainage at the site
-
Fever or chills
-
Any other concerns
Know what problems to watch for and when you need to call your healthcare providers. Also know what number to call after office hours and on weekends and holidays.
Next steps
Before you agree to the test or the procedure, make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how you will get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much you will have to pay for the test or procedure